We have multiple research groups in our department. Basic and clinical
research is conducted in collaboration with a number of research departments
and institutions in each expertise. The following is a brief overview of
the research conducted in our department.
Cerebrovascular Disease
The Tohoku region has a high incidence rate of cerebrovascular diseases such as cerebral infarction, cerebral hemorrhage, and subarachnoid hemorrhage. Research has been actively conducted since the establishment of our department with the aim of improving the quality of life and the functional prognosis of the patients.
In clinical research, the results of a clinical trial for subarachnoid hemorrhage, which was led by Tohoku University, have recently been acknowledged, resulting in the approval of a new drug for clinical use. Additionally, the newly established Tohoku University subarachnoid hemorrhage management protocol, which is compatible with the abovementioned new therapeutic agent, is spreading nationwide. Our research on moyamoya disease, a clinical condition named by our first head professor, Dr. Jiro Suzuki, has kept progressing, and we have reached many impactful findings on changes in cerebral circulation after revascularization surgery for moyamoya disease.
In basic research, we were the first to identify a susceptibility gene for Moyamoya disease, and we are conducting research on it using genetically engineered mice and patient-derived iPS cells. We are making relentless efforts to elucidate the pathogenesis of moyamoya disease, an intractable disease with an unknown cause. Another focus of ours is research on neuroregenerative medicine as a novel treatment for cerebrovascular diseases. As described in detail in the section on regenerative medicine, we work on investigating the detailed mechanisms of therapeutic agents used in said contexts, and their applicability in treating other conditions.
In addition, we are conducting both clinical and basic research on cerebrovascular disorders in general, including dural arteriovenous fistula, cerebral arteriovenous malformation, cervical internal carotid artery stenosis, and endovascular treatment.
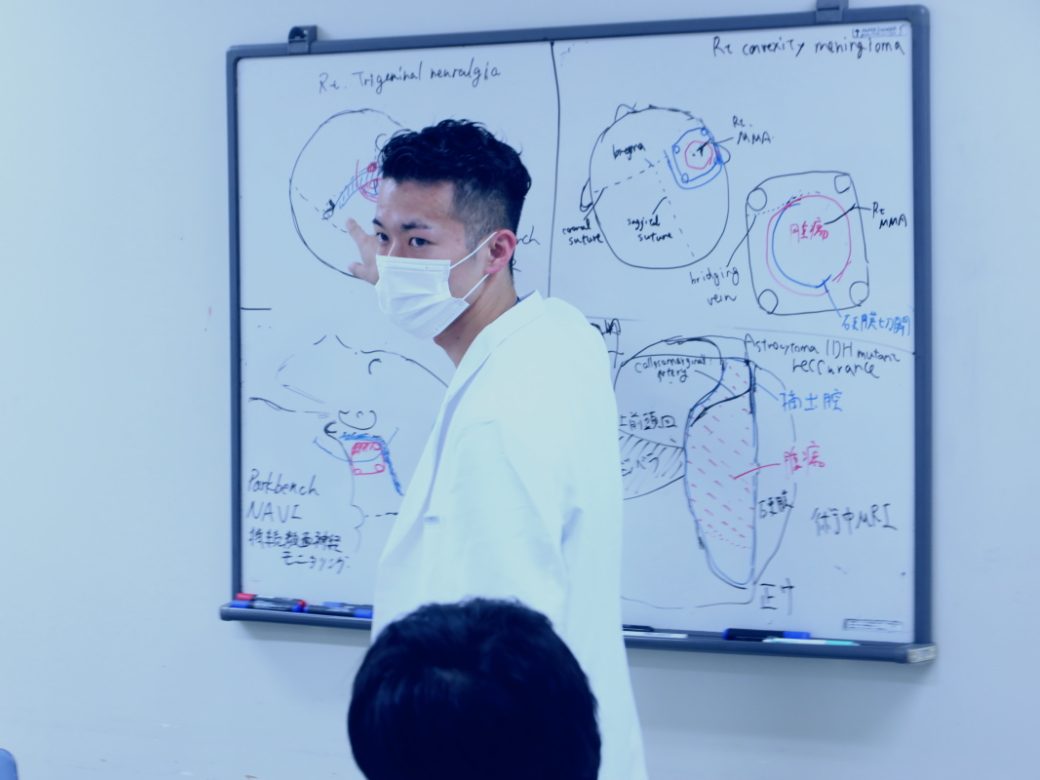
Brain Tumor
We conduct a wide range of research aimed at improving treatment outcomes for patients with brain tumors. With the consent of patients, we conduct genetic analysis of surgically removed brain tumors to analyze the causes and pathology of brain tumors. As a result, we have found that anticancer drugs are highly effective in patients with specific genetic abnormalities, and these results have been applied to treatment.
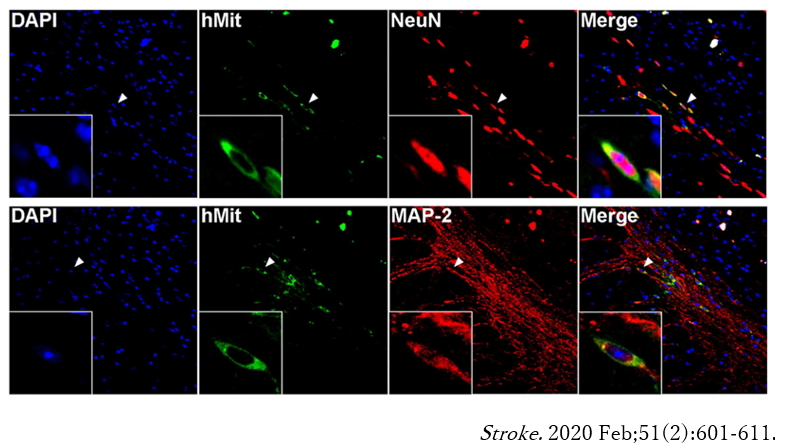
Regenerative Medicine
For decades, stem cell therapy has been sought after as a solution to
treat numerous diseases. MUSE (Multilineage Stress-Enduring) stem cells
are endogenous pluripotent-like stem cells. They are naturally occurring
cells, found in the bone marrow, peripheral blood, and connective tissues
of organs and are thus non-tumorigenic. MUSE stem cells have been discovered
by Professor Mari Dezawa, who is currently a Professor at Tohoku University.
In our lab, we carry out extensive work on the utility of MUSE stem cells
in treating neurological diseases. Our ongoing work focuses on ischemic
and hemorrhagic strokes as well as traumatic brain and spinal cord injuries.
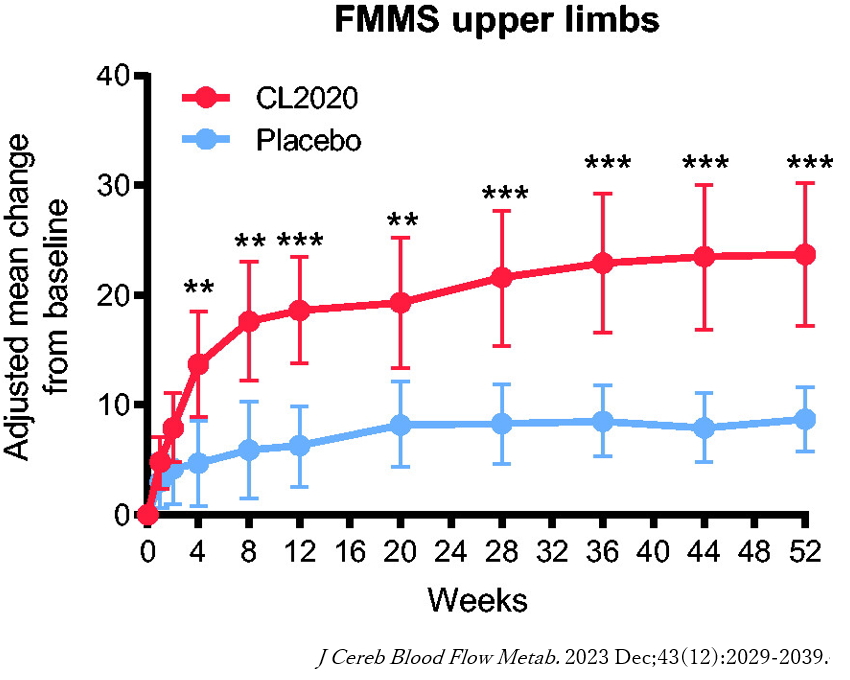
Our department spearheaded a clinical study on the use of MUSE cells in
ischemic stroke (Niizuma et al, JCBFM, 2023). Our ongoing work focuses
on developing novel methods for the preparation and optimization of MUSE
stem cell delivery, the expansion of MUSE cell application to various diseases,
and understanding the basic biology by which MUSE stem cells offer neuroprotective
benefits.
For more information, please visit the Niizuma Lab website.
https://www.neurosci.med.tohoku.ac.jp/en/en-top/
静脈から投与したMuse細胞が脳梗塞に集まり、神経細胞に分化しています。
Muse細胞投与により、脳梗塞患者の上肢麻痺に有意な改善が見られました。
Medical AI
In recent years, the "Medical AI" initiative, which aims to improve the quality of medical care through artificial intelligence (AI), has been spreading rapidly. AI is used in a wide range of fields, including diagnosis, treatment, drug development, and nursing care, but its utilization in the field of diagnostic imaging has seen remarkable progress. Therefore, the use of clinical AI has very strong prospects. In addition to clinical practice, AI is also useful for analyzing experimental data in the field of basic experiments using cells and animals.
In collaboration with Tohoku University Clinical AI, we are conducting research to tackle medical challenges in the field of neurosurgery using AI technology (for more information on Tohoku University Clinical AI, please visit https://www.shp.hosp.tohoku.ac.jp/Clinical_ AI/).
Traumatic Brain Injury
We collaborate with top centers in the field of head trauma, including
the Cerebrospinal Trauma Center at the University of California, San Francisco
and the Walter Reed Army Medical Center/Institute of Research. By making
full use of a broad network including the Cross-disciplinary Biomedical
Engineering Collaboration Platform (http://basic.umin.jp), we are promoting
projects from a broad perspective, especially by taking advantage of the
strengths of our university and focusing on research related to industrialization
and medical policy through problem solving.
Epilepsy Surgery
In collaboration with the Department of Epileptology, the Department of
Pediatric Pathophysiology, the Department of Higher Brain Dysfunction,
and the Department of Diagnostic Radiology, we are conducting research
on new diagnostic techniques, brain function mapping, and surgical treatment
prognosis in epilepsy.
In basic research, we have developed and published the world's first seizure model using light-sensitive ion channels, aiming to elucidate the pathophysiology of epilepsy and its therapeutic application. Optogenetics is a technology to manipulate neural functions using light, and is currently one of the most remarkable fields in the field of neuroscience.
Skull base Surgery
With Tohoku University is recognized as one of the six institutions in Japan for the "Practical Surgical Techniques Training Program" by the Ministry of Health, Labour and Welfare, we conduct surgical-technique training using cadavers and microanatomy training (once a year).
Another one of our focuses is the development of a new surgical treatment device for neuroendoscopic surgery.
Medical Device/Solution Development
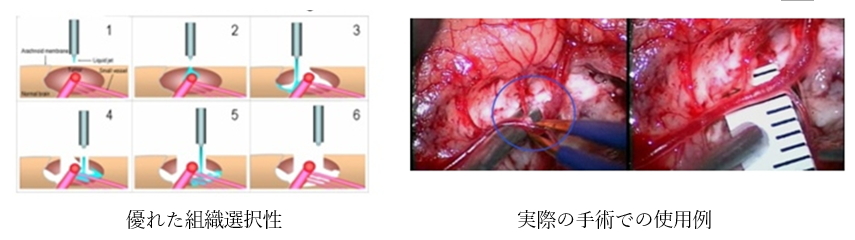
Development of a Surgical Treatment Device (Pulsed Water Jet Scalpel) for Maximum Lesion Extraction with Nerve and Vessel Preservation
http://www.rpip.tohoku.ac.jp/seeds/profile/312/lang:jp/
Surgical procedures require maximum lesion removal from the viewpoint of
maximizing the patient's life expectancy and disease control. On the other
hand, to maintain the patient's function and quality of life after the
surgery or procedure, the blood vessels and nerves in or near the lesion
must be preserved. It has often been difficult to achieve balance between
both. We have focused on the fact that the water jet removes tissue selectivity
without causing thermal damage, and have conducted joint research with
companies and academic institutions to develop a new surgical medical device
(pulsed water jet scalpel) that takes advantage of these two factors, making
it quite effective not only in the field of neurosurgery, but also in various
other fields (spinal cord surgery, gastrointestinal surgery, urology, cardiovascular
surgery, ophthalmology, plastic surgery, dermatology, and dentistry).